by Anne Blythe
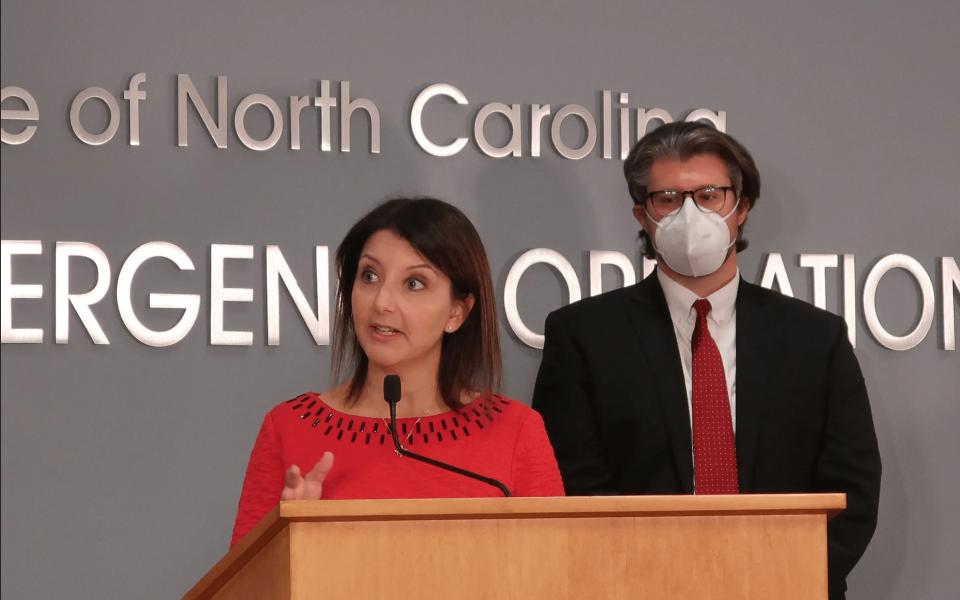
Featured photo: Outgoing health and human services Sec. Mandy Cohen speaks at a broadcast press briefing from the Emergency Operations Center in Raleigh on Monday, Dec. 20, 2021. Behind her stands Kody Kinsley, her replacement as of Jan. 1, 2022. (Photo by NC Health News | Rose Hoban)
The message was dire from Gov. Roy Cooper and Mandy Cohen, secretary of the state Department of Health and Human Services.
“Get boosted,” they repeatedly told North Carolinians on Monday during a briefing with reporters broadcast on PBS North Carolina.
In anticipation of a tremendous surge in COVID-19 cases in early January as the Omicron variant looms large on the horizon, Cohen returned to the Emergency Operations Center podium with a sense of urgency in her last days on the job.
Just a week earlier, Cohen told North Carolinians that she thought her update on the state’s COVID trends, metrics and data would be her final press conference. At the end of the month, she plans to resign from her job and turn over leadership of the state’s pandemic response to Kody Kinsley, the chief deputy secretary at DHHS tapped by Cooper to lead the department as the next secretary of health.
“We thought last week might be your last time at the podium, but this pandemic continues to throw us curveballs,” Cooper told Cohen on Monday after she laid out what she wants North Carolinians to do immediately before Omicron becomes as prevalent here as it is in New York and other parts of the world.
Cohen issued a secretarial advisory on Monday urging all this winter and holiday season to get vaccinated, boosted and tested, and mask up in public places.
COVID cases are on the rise, and North Carolina health care systems are starting to show strain as influenza circulates and the Delta and Omicron variants pose threats.

Cohen and Kinsley said they expected to see record numbers of cases in the peak of the expected Omicron surge. Though Cohen was reluctant to put a specific number on what that record might be, she estimated that it could be as high as 10,000 cases a day. She also declined to speculate what peak hospitalization might look like as a result of the Omicron wave.
North Carolina reported 10,541 new lab-confirmed cases of COVID since Friday, Cooper said. There were 1,630 people hospitalized with severe illness related to COVID, 437 of whom were in intensive care unit beds.
Three days ago, New York reported its highest number of daily COVID cases since the start of the pandemic. North Carolina public health officials are preparing for a similar trend to take hold here in the weeks ahead.
“I have two messages for North Carolinians today,” Cohen said with a more urgent tone in her voice than typical at press briefings. “First, the newest variant of COVID-19, Omicron, is the most contagious we’ve seen yet and will likely set record-high, daily case numbers in the coming weeks. Second, and most importantly. You can act now to best protect yourself and family and friends.”
People who received a Pfizer or Moderna vaccine at least six months ago are eligible for a booster and should get one as soon as possible. Those who received a Johnson & Johnson vaccine are eligible for a booster two months after receiving their shot. They can also get a Pfizer or Moderna shot to boost their immunity.
‘Do not wait’
The Omicron variant, which has been detected in “most” hospital labs across the state, according to Cohen, is two to three times as contagious as the Delta variant, currently the dominant variant in North Carolina.

“Fortunately, early evidence suggests that illness from the Omicron variant may be less severe,” Cohen said. “However, it still can pose a danger for people who are not vaccinated, and particularly those who are at higher risk of severe disease.”
During the week ending Dec. 11, Omicron accounted for 12.9 percent of all cases in the U.S. and 37 percent of cases in the Southeast. By the conclusion of the week ending Dec. 18, updated data from the Centers for Disease Control and Prevention shows that Omicron was accounting for 73.2 percent of all cases in the U.S. and 95.2 percent of all cases in the Southeast (Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, Tennessee).
Instead of throwing hands up in the air, frustrated that the Omicron variant has shown the strength and adaptability of the coronavirus that has disrupted life for 22 months during the pandemic, Cohen urged North Carolinians to take action.
“Do not wait,” Cohen said, stressing each word.
Researchers from Hong Kong found that Omicron reproduces itself up to 70 times more effectively in the upper airway of an infected person than Delta did, making it spread that much more widely when that person coughs or sneezes. The good news is that Omicron doesn’t reproduce as effectively in the lungs, those researchers found. That could be why Omicron appears to cause less severe disease overall, the researchers speculated.
Public health officials in this country, though, say Omicron is too new to the states to predict whether that will remain the case in the weeks ahead.
As health care systems prepare to treat anyone sickened by the Omicron variant, drugs they’ve used in recent months to help stave off severe illness from the previous variants are not likely to offer much help.
‘Diminished’ COVID therapies
Regeneron, a drug company that created monoclonal antibody therapies that can be used for patients at risk of progressing to severe illness, put out a statement that its current drug has “diminished potency versus Omicron.”
New drugs are being developed, but they might not be readily available if an Omicron surge comes as expected in the weeks ahead.
Cohen was asked whether the record number of cases that she expected in North Carolina starting in early January would also mean a record number of hospitalizations.
“I do not yet know what that will translate into in terms of hospitalizations,” Cohen responded. “What we are seeing with Omicron is, it does seem to be less severe. What we don’t know yet is how it’s going to behave here in the United States. With the level of vaccinations that we’ve had, with the kinds of vaccination that we’ve seen before, I don’t know what that will mean. We are certainly planning to see additional strain on our hospitals. That’s why we are working with our hospitals to be ready, and the more we can act right now, that’s what will protect folks.”

“Right now,” though, is four days before Christmas Eve, when many families plan to gather to celebrate the holiday together after being forced to spend it apart in 2020 because of COVID. Some families are reconsidering how they might celebrate the holidays ahead, while others have opted to gather despite the variant.
“I know people are frustrated and dismayed by this wave of infection right here at Christmas, but it’s important to remember how far we have come in our fight against this disease,” Cooper said. “We know what works. Vaccines, boosters, testing and masks when needed. With every dose, we’re getting closer to turning the tide on this sickness and death brought on by the pandemic.”
Cooper said his family is vaccinated and boosted. They plan to get tested, “then gather for food, prayer, presents and hugs and time with each other.”
Testing in the spotlight again
Kinsley outlined what the state has done in anticipation of Omicron. They have gotten boosters to state-run nursing homes and worked with hospitals to build systems to support them as weary workers and understaffed nursing teams add an even thornier layer for health care systems.

Kinsley also said the state is looking ahead to make sure that enough testing supplies are available during the expected surge. Testing for COVID will be a crucial element in schools, businesses and other places.
During the high-water mark of the Delta surge, which occurred in the late summer, North Carolina saw as many as 86,000 tests administered some days.
With public health leaders advising people who plan to gather for the holidays to get tested in advance, a spotlight has been cast again on whether tests are as easy to find as they should be.
Many pharmacies have empty shelves where rapid at-home antigen tests once were stocked. Even if the shelves were stocked, at nearly $25 a box for some brands with only two tests included, the cost of home testing can add up quickly.
Kinsley stressed that free home-testing is available in North Carolina through DHHS. They’re not the rapid antigen tests, though. The swabs must be sent to a lab to get PCR results, adding a step that could lead to a delay in results.
“Over the last several weeks we’ve pushed out several hundreds of thousands of tests, rapid tests, to our local health departments to make them available in local communities,” Kinsley said. “Of course we have statewide testing vendors that are providing testing in schools.”
Coronavirus by the numbers
According to NCDHHS data, as of Monday afternoon:
- 19,167 people total in North Carolina have died of coronavirus.
- 1,599,595 have been diagnosed with the disease. Of those, 1,630 are in the hospital. The hospitalization figure is a snapshot of people hospitalized with COVID-19 infections on a given day and does not represent all of the North Carolinians who may have been in the hospital throughout the course of the epidemic.
- As of Tuesday, 437 COVID-19 patients were in intensive care units across the state.
- North Carolina tracked COVID-19 re-infections in the case counts from March 1, 2021 through Sept. 20, 2021. All told, North Carolina tracked 10,812 reinfections, 200 of those were in people who were previously vaccinated. Ninety-four people who were reinfected with COVID-19 have died.
- 1,538,231 people who had COVID-19 are presumed to have recovered. This weekly estimate does not denote how many of the diagnosed cases in the state are still infectious. Nor does it reflect the number of so-called “long-COVID” survivors who continue to feel the effects of the disease beyond the defined “recovery” period.
- To date, 21,190,766 tests have been completed in North Carolina. As of July 2020, all labs in the state are required to report both their positive and negative test results to the lab, so that figure includes all of the COVID-19 tests performed in the state. Most recently, 9.3 percent of those testing were testing positive.
- People ages 25-49 make up the largest group of cases (39 percent). While 12 percent of the positive diagnoses were in people ages 65 and older, seniors make up 74 percent of coronavirus deaths in the state.
- 263 outbreaks are ongoing in group facilities across the state, including nursing homes and correctional and residential care facilities.
- As of Dec. 20, 6,539,752 North Carolinians have received at least one dose of a coronavirus vaccine. Ninety-one percent of people over the age of 65 have been completely vaccinated, while 58 percent of the total population is fully vaccinated. 2,184,783 boosters have been administered.
- Children between the ages of 5 and 11 became eligible for vaccination during November. A total of 161,410 first doses have been given to those children, a total of 18 percent of that population.
This story has been updated with new data from the Centers for Disease Control and Prevention.
This article first appeared on North Carolina Health News and is republished here under a Creative Commons license. North Carolina Health News is an independent, non-partisan, not-for-profit, statewide news organization dedicated to covering all things health care in North Carolina. Visit NCHN at northcarolinahealthnews.org.
Join the First Amendment Society, a membership that goes directly to funding TCB‘s newsroom.
We believe that reporting can save the world.
The TCB First Amendment Society recognizes the vital role of a free, unfettered press with a bundling of local experiences designed to build community, and unique engagements with our newsroom that will help you understand, and shape, local journalism’s critical role in uplifting the people in our cities.
All revenue goes directly into the newsroom as reporters’ salaries and freelance commissions.

Leave a Reply